Healthcare-acquired infections (HAIs) are also known as nosocomial infections and are as a result of the transmission of an infection to a patient who is receiving medical or surgical care while in a healthcare session such as a hospital, surgical facility, ambulatory facility or long-term nursing home or rehabilitation center. These infections are not present in the patient before they enter a hospital facility for treatment.
While HAIs are a risk for any patient that is being cared for in one of these facilities, young children, the elderly and those with compromised immunity may be more susceptible to these nosocomial infections. Patients who remain in these facilities on a long-term basis or who require catheterization, are also more susceptible to infections. Additional risks include the over prescription of antibiotics and healthcare providers who may not adhere to strict infection control practices, such as washing their hands between patient interactions.
Intensive care units are among the most common areas of the hospital at highest risk for HAIs, and it is suspected that around 1 in 10 people who are admitted will be infected with an HAI. Around 1.7 million infections take place every year, which cause approximately 99,000 annual deaths (1).

Infections can be caused by bacteria, viruses, and fungi, with bacteria being proposed as contributing to around 90% of all HAIs. Five of the most common types of HAI are:
1. UTIs
2. Infections of surgical sites
3. Gastroenteritis
4. Meningitis
5. Pneumonia
More recently, we have dealt with the sudden exposure to a new threat: the 2019 novel coronavirus. While research is still being conducted as to the state rate of infection, it has been made clear that it may be one of the deadliest HAIs of this decade.
COVID-19 is primarily transmitted through respiratory droplets (2), which poses a serious threat to the intra-hospital environment for healthcare workers and patients alike.
Maintaining strict hygiene standards, wearing the appropriate protective personal equipment (PPE), restricting access to facilities and isolating patients who are positive or are suspected of having the virus are some of the measures currently in place to reduce the risk of intra-hospital transmissions (3).
Much of the infection control practices that have been put in place since the start of the pandemic, reflect on the protocols used in previous pandemic outbreaks, such as the 2003 SARS pandemic.

HIGH RISK ENVIRONMENTS IN HEALTHCARE FACILITIES
The patient environment within a healthcare facility plays one of the most important roles in transmission of HAIs (4).
Contamination occurs from an infected patient via three major routes:

The patient themselves and the microorganisms they harbor, which may translocate onto bedding and other textiles that they are in direct contact with.

They transmit organisms directly onto surfaces they come into contact with, including floors.

There is contamination of the equipment that is used in their care.
In a large-scale study, the risk of developing a HAI was determined over the course of seven years in four hospitals. The findings of the study indicated that a patient has a six times greater risk of developing a HAI when a prior bed occupant had positive colonization, and a five times greater risk if they had been the roommate of a positively colonized patient (5).
The prevention of HAIs lies with the healthcare facility and all of those who work in them. Adherence to strict prevention control practices has been shown to reduce the risk of transmission of infections in hospital settings by more than 70%.
Four important recommendations to follow include:

Healthcare workers need to wash their hands at regular intervals with soap and water or, preferably, an specialized hand sanitizing rub. Hand cleaning practices need to be performed at least before and after interactions with each patient.

When a patient requires catheterization, the area of the site should be cleaned, and sterilized equipment used. The catheter should only remain inserted in the patient for the maximum intended time of treatment and removed as soon as possible.

Where appropriate, healthcare workers should wear personal protective equipment such as hair covers, face masks, gowns and gloves, some of which may need to be changed in between patients.

Taking care to ensure surfaces are cleaned thoroughly and regularly and that rooms are kept well ventilated, with air filtration systems in place, where possible.
In summary, infection control and prevention may be achieved through:
Highly specialized products and devices are available to assist in these areas of infection control and HAI prevention.• Standard precautions
• Maintaining proper hand hygiene
• Use of personal protective equipment
• Regular cleaning and disinfection
• Respiratory hygiene and coughing etiquette
TECHNOLOGICAL ADVANCES IN INFECTION CONTROL PRACTICES
Continuous, safe and effective surface and air disinfection lungs.
Over the last 15 years, cleaning and disinfection tactics have taken a quantum leap. In 2005, surface cleaning was generally done by hand with rags and buckets filled with soapy water. The trouble with these methods, however, were that the surface only appeared clean to the naked eye. There was little to no disinfection of potential microorganisms, and they remained a threat to those who came into close contact with the surfaces.
A couple of years later, outcomes of disinfection practices of surfaces improved with the introduction of bleach-containing
wipes. Fast forward 10 years and we are now looking at systems that provide continuous, whole cleaning technology.
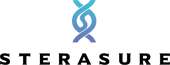
With the CASPR system, it is installed directly into the HVAC system. While there is airflow through the HVAC, the CASPR system will continue to disinfect the environment, including any surfaces that are contained in that space. No longer is it necessary to require a person to clean and disinfect a room, or rely on devices that provide intermittent disinfection.
With the CASPR system, there is total peace of mind, knowing that the system is working behind the scenes, with the entire environment being continuously disinfected.
This is the only product on the market that settles on surfaces, it is guaranteed to address those hard to reach areas and cover every corner of a room that may otherwise be ignored.
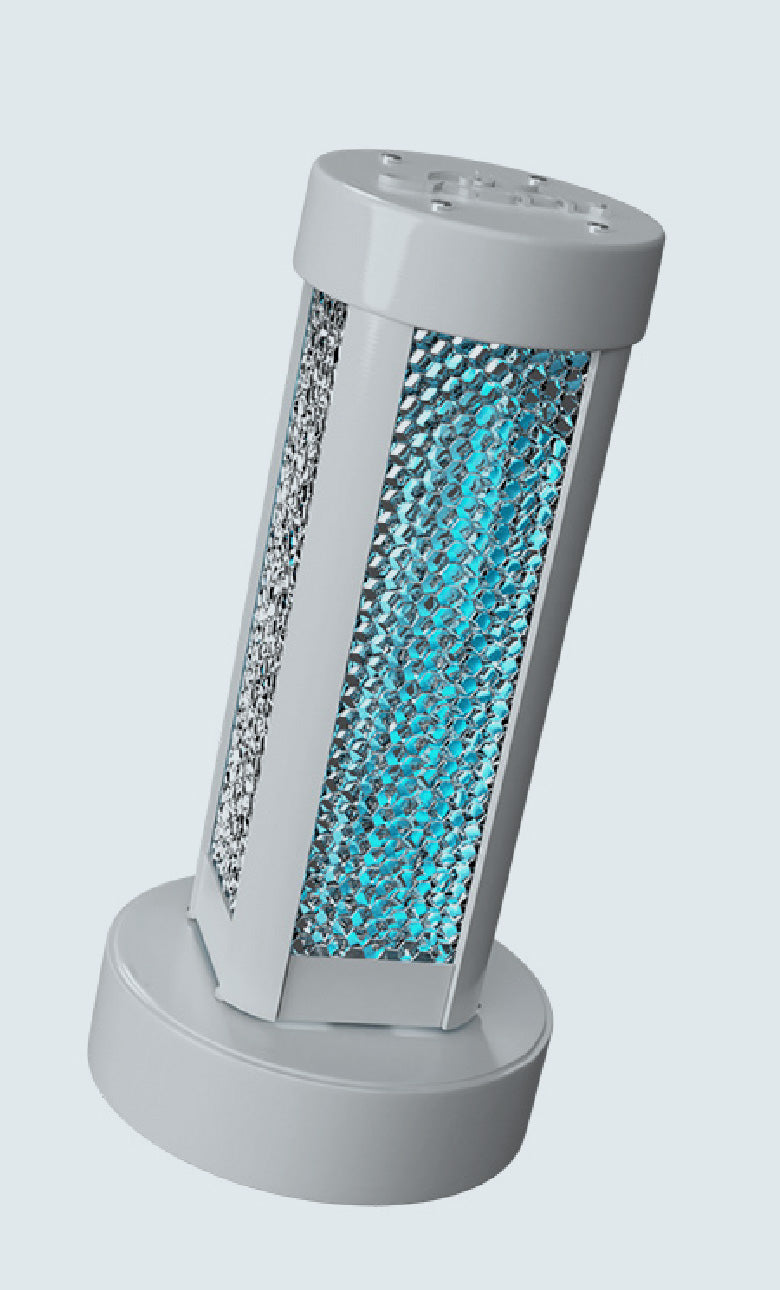
Every surface in the environment in which it is installed is completely disinfected from potential life-threatening microorganisms, including the family of coronavirus pathogens.
It has been well-documented that the inanimate hospital environment poses high risk of contamination with nosocomial pathogens. Compelling evidence shows that pathogens such as Clostridium difficile, vancomycin-resistant enterococci, and methicillin-resistant Staphylococcus aureus are highly likely to contaminate surfaces within these facilities, which poses a risk of indirect cross-contamination. It has also been proposed that there is probable survival of other pathogenic microorganisms such as norovirus, influenza virus, severe acute respiratory syndrome-associated coronavirus, and Candida species on surfaces, which indicates the dire need to place emphasis on their cleaning and disinfection (6).
Current technology involves periodic cleaning of the environment. A system or device may clean a room on a set schedule, for example, however, an infectious person may enter the room following the cleaning cycle, which leaves other people entering the room at just as great a risk as before.
Indeed, a 2018 study7 has shown that despite cleaning of a room at the end of a patient’s stay, 55% were found to be contaminated with a multidrug-resistant organism (MDRO) when samples were taken following a new patient admission. While the samples contained lower levels of microorganisms, the risk of cross-contamination and likelihood of HIA remained high.
In general, surfaces healthcare facilities that need to be considered as a likely source of cross-contamination include (8):

Wards and patient rooms including all areas that a patient may come into contact with, as well as patient charts and records.

Linens in direct contact with the patient as well as all of the textiles that may be used in the hospital environment, including curtains and/or blinds.

Crash carts and procedure trays as well as all diagnostic equipment

Nursing stations and the set up of computer and keyboards as well as patient files
Many of these surfaces may be missed as a source of cross-contamination when addressing the cleaning and disinfecting of surfaces.
It has been documented that adequate cleaning of the hospital environment is lacking9. In Canadian hospitals, almost 50% of environmental services managers have reported adequate staff to satisfactorily clean their hospitals. Shortages of cleaning personnel and cost-saving measures may result in reduced cleaning frequency of the environment and all of the elements that require regular cleaning and disinfection. Solutions used may themselves be inadequate due to over dilution and insufficient contact time with the surface, for example.
CASPR offers a solution for the removal of the human element responsible for disinfecting the hospital environment (10).
The CASPR device provides a true “no-touch” technology for cleaning and disinfecting any internal environment through a natural photocatalytic converter system that converts air and water into oxidizing molecules.
These molecules are dispersed through the air, effectively and safely covering surfaces across the area in which it has been installed, working continuously to reduce the burden of microorganisms that are responsible for HAIs in the hospital setting.
Odors are also eliminated when using this system and it is completely safe to use on a continuous basis, even in occupied spaces.
In trials conducted in hospitals, the CASPR system was demonstrated as having the following effects.
In Oklahoma hospitals:
• >98% reduction in bacteria on high-touch surfaces
• >90% reduction in the average fungal spores
• 93% reduction of positive MRSA infected-surfaces
In Iowa hospitals:
• 8-10 fold decrease of microorganisms in hospital rooms, at nurses stations and contained within targeted textiles
• Elimination for the need of UV light decontamination systems
• Improved room turnover by more than 30 minutes
• 42% reduction in staff absenteeism
From a hospital standpoint, this is a critical device to consider, which may save millions of lives through the significant reduction - and potential elimination - of the risk of HAIs for anyone who enters one of these medical facilities, be it patient, their family members or a healthcare worker.
HYPOCHLOROUS ACID-CONTAINING DISINFECTANT SPRAY
FOR THE USE AS A PERSONAL SANITIZER, GENERAL DISINFECTANT, WOUND CARE AND DEBRIDEMENT
One of the most effective chlorine-based disinfection solutions contains the natural biochemical hypochlorous acid. HOCl is produced in the human body by granulocytes as a result of pathogenic stimulation of the immune cascade.
Previous attempts to create a HOCl solution have failed, however, the recent development of a pure HOCl solution has revolutionized the technology, providing a safe, highly effective topical antimicrobial product, as an alternative to waterless alcohol-based hand sanitizers. Briotech, which contains the pure BrioHOCl, has been shown to be highly effective at eliminating viruses, bacteria, endospores, fungi and prions on the surface of the skin without irritation, even when used on mucous membranes, the eyes and open wounds.

Research has shown that it clears 95% biofilms within 5 contact minutes and degrades to water with low-concentration NaCl within 30 minutes, without persistent residue or hazardous waste.
This safe, effective and affordable disinfectant spray may prove highly beneficial to healthcare providers in the hospital setting, not only for personal infection control, but for use on surfaces, and patients who may have varying requirements.
Open wounds pose a high risk of infection, particularly to patients who are already vulnerable, such as those in long-term care facilities. Infection of wounds is well known to result in increased mortality rate, loss of function, loss of quality of life and increased pain.
BrioHOCl, however, can be applied directly to the area of broken skin, surgical sites and to mucous membranes with proven ability to reduce microorganism aggregation and in doing so, lowering the risk of infection and its serious consequences.
BrioHOCl can also be used for personal sanitization.
It has been estimated that around 20-40% of HAIs are due to the cross-contamination resulting from microorganisms on the hands of healthcare workers (11). These infections come from infected patients, other healthcare workers or through direct contact with a contaminated surface and they then cause further direct contact contamination when transmitted to other healthcare workers, patients and even inanimate objects in their immediate environment (12).
HOCl has also been shown to be effective in cleaning hospital rooms, where a fog of HOCl effectively eradicated C. diff within a very brief exposure time. Additional research findings also provide evidence for the use of an HOCl solution in the elimination of persistent norovirus infections within 10 minutes of contact, legionella reduced to non-detectable levels following an HOCl misting, and the eradication of avian influenza in 10 seconds or less.
Importantly, the safety profile of pure HOCl is high, where findings show that inhalation of BrioHOCl causes no adverse effect and, in fact, is being evaluated in its application as a therapeutic agent for nebulization to patients with respiratory tract infections.
UV TECHNOLOGIES TO REDUCE THE RISK OF HOSPITAL ACQUIRED INFECTIONS
UV SMART TECHNOLOGY
Another no-touch technology that has been well studied in room and surface disinfection is the incorporation of devices that utilize UV emission (13). UV irradiation has been shown to break down molecular bonds in the DNA of microorganisms.

While the type of UV device may alter the findings, one study showed that (14):
• The use of a UV device for 15-20 minutes had a significant effect on vegetative bacteria such as MRSA.
• C. diff spores, while requiring extended exposure to UV of between 35-100 minutes, were significantly decreased on contaminated surfaces.
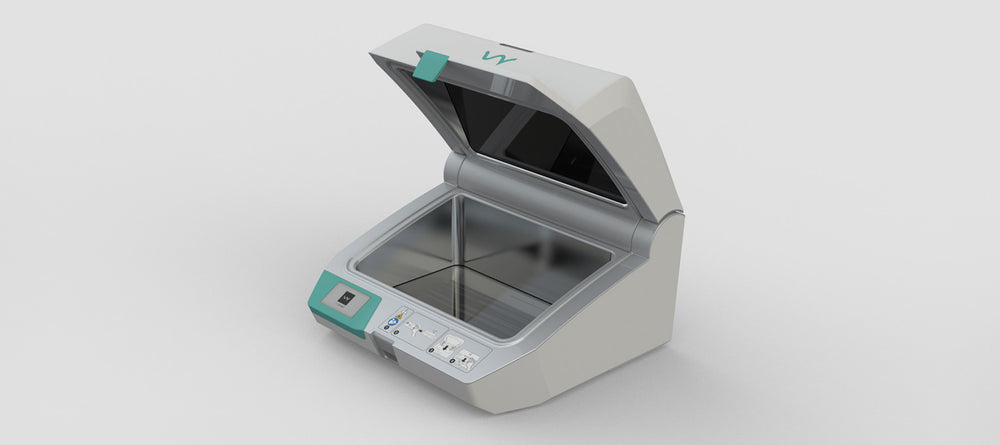
UV Smart offers an emergency version of a UV light device that may be used to clean and disinfect those items medical personnel may need to reuse when caring for patients back-to-back.
A healthcare provider may have the need for multiple N95 masks, for example, switching out the device in between treating patients that have a known or suspected respiratory infection, such as COVID-19.
In the past few months, during the outbreak of COVID-19, scarcity of PPE and mouth-nose masks has been a major concern for many healthcare workers.
While these masks are typically made for single use, in an event of an emergency, the UV smart may reduce the need for a new mask - provided it is not visibly soiled or contaminated - as it provides a quick and easy solution for disinfecting these masks.
It uses powerful, contained UV technology that has been shown to disinfect medical devices such as masks, which allows them to be reused and continue to provide adequate protection, without increasing the risk of infection to both provider and patient.

The respirator may be placed into the UV light container, which uses Impelux technology to disinfect items in as little as 50 seconds. Not only is the device easy to use and it offers an incredibly fast cycle of disinfection, there has been no report of damage to materials that have been placed within the container, and there is no outward risk of radiation when the device is in progress. The UV Smart device requires no chemicals or solution-based disinfectants. Within 25-100 seconds, an array of reusable medical devices and multiple PPE can be placed directly into the UV smart container, and disinfected in the time it takes the healthcare provider to wash their hands.
With thousands of people dying from HAIs every year in Northern America alone, there really is a serious need for improved infection control practices. Should there be little in the way of staffing availability to meet these needs, particularly like we have seen in times such as the COVID-19 pandemic, we need to look towards technological advances that offer help.
From complete and continuous air and surface purification with the CASPR device, spray on disinfectants such as the Briotech, or a UV light container like the UV Smart, not only can technology ease the burden on environmental service workers, it improves the working environment of healthcare providers, allowing them to focus on what’s most important; their patients. And of course, improved and more targeted infection control practices have a significant impact on the health and wellbeing of all patients no matter the hospital or medical facility they rely on for their care or treatment.
REFERENCES:
1. Klevens R., et al. Estimating Health Care-Associated Infections and Deaths in U.S. Hospitals, 2002. Public Health Reports 2007; 122: 160-166.
2. Peeri N., et al. The SARS, MERS and novel Coronavirus (COVID-19) epidemics, the newest and biggest global health threats: what lessons have we learned? Int J Epidemiol. 2020 Feb 22.
3. Gan, W., et al. Preventing Intra-hospital Infection and Transmission of Coronavirus Disease 2019 in Health-care Workers. Saf Health Work. 2020 Mar 24.
4. Suleyman G, Alangaden G, Bardossy AC. The role of the environmental contamination in the transmission of nosocomial pathogens and healthcare-associated infections. Curr Infections Dis Rep 2018;20:11-12.
5. Cohen B., et al. Association between healthcare-associated infection and exposure to hospital roommates and previous bed occupants with the same organism. Infect Control Hosp Epidemiol. 2018;39:541-46.
6. Weinstein, R., & Hota, B. Contamination, Disinfection, and Cross-Colonization: Are Hospital Surfaces Reservoirs for Nosocomial Infection? Clinical Infectious Diseases. 2004. 39(8):1182–1189.
7. Chen L., et al. A prospective study of transmission of multidrug-resistant organisms (MDROs) between environmental sites and hospitalized patients – the TransFER study. Infect Control Hosp Epidemiol. 2018;40:47-52.
8. Harbath S., et al The preventable proportion of nosocomial infections: an overview of published reports. J Hosp Infect. 2003;54:258-266.
9. Zoutman DE, Ford BD, Sophia K. Environmental cleaning resources and activities in Canadian acute care hospitals. Am J Infect Control 2014;42:490-4.
10. Carling PC., et al. Healthcare Environmental Hygiene Study Group. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infect Control Hosp Epidemiol. 2008;29:1-7.
11. Randle J, Arthur A, Vaughn N. Twenty-four hour observational study of hospital hand hygiene compliance. J Hosp Infect 2010;76:252-5.
12. Stiefel U., et al. Contamination of hands with methicillin-resistant Staphylococcus aureus after contact with the skin of colonized patients. Infect Control Hosp Epidemiol 2011;32:185-7.
13. Rutala WA, Gergen MF, Weber DJ. Room decontamination by ultraviolet radiation. Infect Control Hosp Epidemiol 2010;31:1025-9.
14. Boyce J., et al. Impact of room location on UV-C irradiance and UV-C dosage and antimicrobial effect delivered by a mobile UV-C light device. Infect Control Hosp Epidemiol 2016;37:667-72.