Aesthetic therapies have become increasingly popular over the last few years, with many people seeking interventions that defy the effects of ageing. Some of the most common procedures include botulinum toxin injection, or botox, microneedling and collagen therapy, chemical peeling, laser therapy, radiofrequency, various forms of facelift procedures, and fat reduction or redistribution. Many of these procedures have high safety profiles, however, whether it’s a tiny puncture or a large incision, aesthetic procedures cause some form of injury to the skin, which is always associated with some level of risk (1).
With the skin being one of the largest organs in the body, providing a barrier function against infection, breaches in its integrity, no matter how small, poses a risk for the infiltration of microorganisms and subsequent risk of infection.
To increase the rate of positive outcomes following aesthetic procedures, optimal wound healing is required. One of the elements to consider in this regard is the maintenance of aseptic techniques, with high adherence to sterile practises, before, during, and continuing after the procedure. Unfortunately, it has been seen that many clinicians or aesthetic technicians are not aware of the severe nature of complications that may arise from seemingly minimally invasive procedures (2).

Infection not only poses a risk to the overall outcome of the procedure; infection increases the risk of scarring, which has serious implications to the patient, most significantly, to their mental health and wellbeing.
POPULARITY OF COMMON AESTHETIC PROCEDURES MAY POSE A THREAT TO ASEPTIC TECHNIQUES
Sub Heading goes here
One of the concerns in the medical aesthetic industry is the influx of non-medical technicians who may not have the clinical experience or set of skills that are required to be able to fully understand the need for aseptic techniques, which are critical for infection prevention and control.
It has also been written that nurses have created business opportunities where they provide treatments to patients in more convenient locations, such as in their own home or office, in a hotel room, or any other environment that is not one that has been well-managed to adhere to strict hygiene standards.
The serious nature of a risk of infection should be reinforced throughout all of the medical aesthetic industry, and all providers, be they medical or non-medical technicians.
Careful consideration of the risk of infection and adherence to aseptic techniques needs to remain an essential part of the business structure alongside the projection of the image of the center, in the hopes of attracting new clients (3).

THE RISK OF INFECTION IN AESTHETIC CLINICS
Four major areas of concern that may cause transmission of microorganisms in the aesthetic industry are:

Physical contact between a provider and client may allow for transmission of microorganisms if aseptic techniques are not adhered to. Additionally, a provider or client may contaminate a surface, which increases the risk of cross-transmission to other providers or clients.

A provider or client who coughs, sneezes or even talks loudly may be responsible for the release of contaminated droplets into the air. These larger droplets may be suspended for only a short period of time, however, may also contaminate nearby surfaces.

Smaller droplets may be suspended in the air for long periods of time, increasing the risk of inhalation and cross-transmission to many more people who enter the environment.

When aseptic techniques break down, medical devices may become a vehicle through which transmission of microorganisms becomes possible.
An extensive amount of research has also been conducted into the role of biofilm formation in the field of aesthetic medicine. Previously, adverse reactions to fillers, in particularly, were thought to occur as a result of immune-regulated reactions. It is now more widely believed that adverse reactions as a result of dermal filler procedures, may indeed be linked to infection.
Research into hyaluronic acid-based fillers are the most popular as non-permanent injectable materials that target specific soft-tissue aspects in the face. Infection, in particular, as a result of exposure to bacteria, is increasingly receiving attention in these HA-filler procedures. In many patients who have developed adverse outcomes, it has been shown that bacteria have produced biofilms, which are aggregates or clusters of bacteria that have formed a protective structure or matrix around their colony. This matrix is highly impermeable to many antibiotics, which poses a significant problem for treatment of these reactions.

Biofilms are slow growing, which makes them extremely difficult to identify; culture tests often come back negative as a result, which further reduces the likelihood of the appropriate treatment. Biofilms have also been shown to be one of the major reasons for the delay in complications that may be seen long after a dermal filler has been injected (4).
Overall, infection control in aesthetic treatment should be made top priority to both improve outcomes for patients, and reduce the risk of adverse effects.
PREVENTING INFECTION DURING AESTHETIC PROCEDURES
WOUND CARE AND ACUTE AND CHRONIC INFECTION CONTROL
Infection control following an aesthetic procedure is essential to not only achieve the benefits the client is hoping for, but to prevent adverse reactions and scarring (5).
While many cosmetic procedures do not produce a significant surgical or traumatic breach of the skin, many of them would produce enough tissue damage through piercing or puncturing the skin that would stimulate the body’s natural healing effect to restore skin barrier function and prevent infection.
During the skin healing process, as the wound closes, it is highly susceptible to environmental and physiological stress factors, as well as infection (6). Interruption of the skin’s natural healing process may lead to persistent inflammation and even pose higher risk of developing scar tissue(7).

Topical antimicrobial agents play a significant role in wound healing following aesthetic procedures. It has been well documented that an optional environment for healing to take place is one where the moisture in the area is maintained, and it is kept clear of debris and microorganisms that may cause infection. Current disinfectants such as iodine and chlorhexidine (CHX) have been widely used , however, they are both considered weak poisons. In higher concentrations, they may damage tissues; at lower concentrations they may not be able to fully eradicate harmful bacteria, viruses or other microorganisms. Additionally, their use is not recommended in exposed tissue, in the eye or other areas where there are mucous membranes. While iodine remains one of the mostly widely used solutions in medical practice, it is well known to cause skin irritation, which along with skin staining, poses a challenge to its use in aesthetic application. CHX is commonly used in aesthetic procedures due to its effectiveness as a broad-spectrum antimicrobial that has low irritant properties. CHX, however, is ineffective against polio virus and adenovirus, and is not considered a sporicidal. Additional challenges for the use of CHX is the high susceptibility of some people to anaphylactic reactions to it, it’s low efficacy against MRSA and Klebsiella pneumonia (8).
Briotech, which is a pure hypochlorous acid (HOCl) solution, has been well-tested in its antimicrobial effects in a hospital setting (9).
HOCl is an old discovery that has been given a 21st century overhaul. Previous attempts to produce it as a disinfectant have been unsuccessful until recent advances having been able to purify the solution, rendering it not only non-toxic, but highly effective as a disinfectant agent. Rendering to water and hydrogen molecules with a low NaCl concentration within 30 minutes, Briotech poses no threat to healing or replicating cells during the wound healing process.
Additionally, HOCl has also been shown to be effective at disrupting biofilms (10). One of the best ways to prevent the risk of biofilm development is by pre-treating the procedure site with an appropriate solution (11).
Being completely safe to apply directly to open wounds and mucous membranes, BrioHOCl rapidly kills bacteria, fungi, viruses and spores while remaining neutral to skin pH and improving blood flow to the area, which stimulates improved skin healing. Within 30 minutes, the solution breaks down to a water solution with a moderate amount of NaCl; no toxic residue or need to rinse.

BrioHOCl has a broad range of uses in the aesthetic industry; it can be used immediately pre- and post-procedure, and can be dispensed to allow for at-home use to reduce the risk of infection on procedure sites.
SURFACE AND AIR DISINFECTION
In any location where there is a high turnover of people entering and leaving the environment, there is a risk of cross-transmission of infection.
With the world having been recently thrown in amidst a serious airborne viral pandemic, it has become even more important to consider the real risk of infection in the aesthetic service environment, not only during treatments and procedures, but in the clinic or offices themselves.
Surfaces and the air pose a significant risk of cross-contamination of microorganisms.
Research has shown that in a confined environment, droplets that contain microorganisms may be a potential source of infection, and they pose a risk to both practitioner and patient. These droplets of varying size may be spread through the aesthetic clinic environment via talking loudly, coughing or sneezing. Smaller microdroplets have been shown to remain suspended in the air for hours, while larger droplets may settle on nearby surfaces (12).
Microdroplets may pose a serious risk of cross-transmission of infection. A person who was in the environment hours prior may infect a person entering the same environment at a later stage, inhaling these suspended droplets that may contain microorganisms.
Adequately ventilated spaces pose less of a problem. However, the type of ventilation also plays a role in the effect in the space. Typical HVAC and other air conditioning units may circulate the air, not actually getting rid of potentially infectious droplets. Ideally, a specialized air filtration system is needed, where the air is not only recycled, but disinfected.
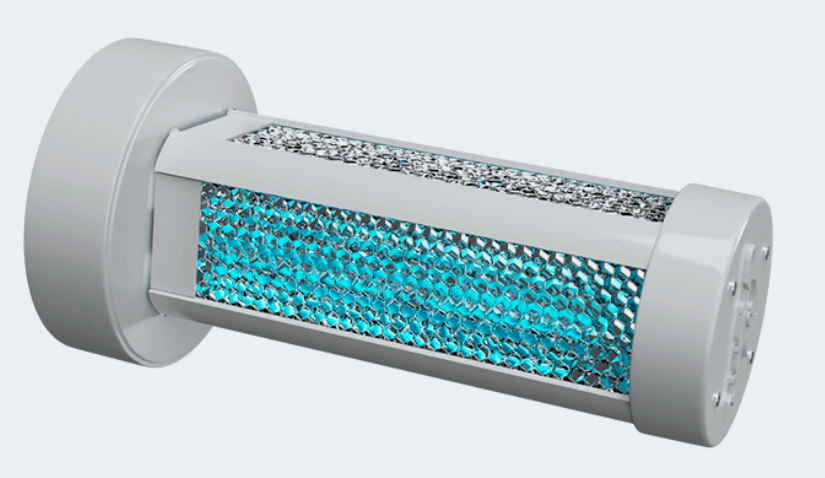
The Light Progress system offers a solution. Not only is air continuously drawn in, processed and filtered, the UV-C device effectively kills microorganism as it passes through the light box. This type of UV-C air filtering device is currently being used in a number of industries that are at high risk of airborne infections such as inside the locker rooms of prominent Canadian sports teams, in daycare centers and hospitals.
Studies that have been conducted on these types of combined filtering and air purification systems have shown that they are capable of eliminating microbial compounds in the air in totality, resulting in 99.9% clean air. The active component of the device is the germicidal box, which contains titanium dioxide, a chemical well known for its effect on both organic and inorganic substances. It works by disrupting the membrane of microorganisms while eliminating noxious odors and gasses such as ammonia and sulfur that they may release. In addition, the UV-C lamps that are contained within the device, further inhibit microbial growth and, due to the reflection that they provide, enhances the germicidal power of the purification system.
The light progress has been shown to be effective against the Avian Flu Virus (H5N1), SARS, Influenza, Herpes, Legionella pneumophila, TB and also infections that may develop as a result of yeasts, molds and fungi that may be inhaled from the air, which are some of the most common airborne infections that are known risks in clinical settings.

Now, the HVAC system in the aesthetic environment may still come in handy. It offers a solution to infection control in its own unique way. By installing a device called CASPR, right into the HVAC unit, additionally disinfection of the environment becomes a breeze.
The CAPSR, which converts water and hydrogen molecules into oxidizing compounds, provides a true ‘no-touch’ disinfection solution. It addresses the multiple gaps in the industry, which relies heavily on available service technicians, who are responsible for cleaning and disinfecting procedure rooms and common spaces used in the aesthetic environment. Not only does periodic cleaning and disinfecting cause delays in the ability of practitioners to perform continuous procedures, appropriate disinfectant solutions may be costly, they may require multiple levels of application, they may be offensive to sensitive groups of people, and overall, not be effective enough for keeping many hard-to-reach areas, or complex surfaces, such as buttons, drawers, and switches, for example, free from germs (13).
Studies conducted in Oklahoma and Iowa hospitals revealed significant reduction in bacteria on high-touch surfaces. Fungal spores and MRSA were reduced on average 90% and 93% respectively. Samples collected in CASPR environments showed an 8-10 fold reduction of microorganism in common areas and on textiles such as curtains and linen, it proved to eliminate the need for UV light decontamination systems, and staff absenteeism was reduced by 42%.
With CASPR, disinfection is continuous. As long as the HVAC remains on, it can provide 24/7 coverage, even in occupied spaces. The oxidizing particles have been shown to effectively break down the cells of a broad spectrum of clinical pathogens, while being non-toxic to humans, and having no effect on the surfaces they land on.
It’s a device that offers peace of mind knowing that focus can be placed on the client or patient and their needs, in a clean and sterile environment that encourages the best outcomes following their procedure.
With added benefits for technicians and practitioners, there’s little question as to whether purified air and environment disinfection should be one of the top priorities in the aesthetic industry.
REUSABLE AESTHETIC DEVICES THAT REQUIRE FREQUENT DISINFECTION
Many multiple use items in the aesthetic practice may need to be disinfected. Probes, extractors, and tweezers, for example, need to be appropriately cleaned between each client to prevent cross-contamination of microbes.

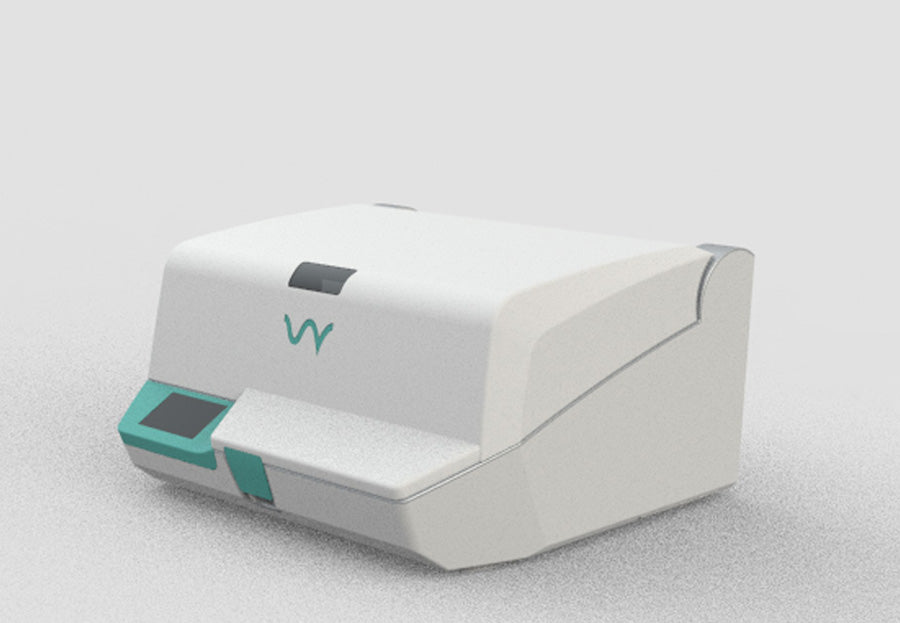
The UV smart device, which uses UV light in a closed container, offers an easy and effective solution to disinfecting small, reusable aesthetic practice equipment.
The device has been shown to kill microorganisms on multiple contaminated items that have been used in clinical practice and in everyday life without changing any feature of the item.
For example, N95 masks, which have been in short supply during the pandemic, have been shown to be effectively disinfected using the UV Smart device, provided they are not visibly soiled. Mobile phones have also been tested in the device, without harmful effects to their materials or function resulting from their UV-C exposure to disinfection.
UV light has long been used in the clinical setting for infection control.
UV-C light is germicidal, causing disruption to the protein cell walls of organisms, and causing cell death of the organism. While highly effective, currently available UV devices, however, pose various challenges due to the risk of human exposure to UV rays, thus being restricted to use in unoccupied environments, and the time required to move the light device into direct line of sight across surfaces that need to be disinfected.
The UV Smart device not only contains the UV light within its internal structure, the Impelux technology ensures consistent and repeatable disinfection from multiple organisms, including SARSCoV1.
The UV-C in the UV Smart device provides 5log, high level disinfection that takes place within 25 to 100 seconds; far quicker than a practitioner would need to prepare for their next procedure or wash their hands.
GENERAL INFECTION CONTROL
Additional infection control practices need to be adhered to:
• Frequent hand-washing with water and soap or appropriate sanitizers, for example, Briotech, particularly following contact with a client or patient.
• Appropriate PPE needs to be worn while the procedures are being performed.
• Equipment needs to be appropriately disinfected and sterilized.
• Follow the instructions for single-use devices appropriately.
• Contain waste and dispose of it in a responsible manner.
Without a high regard towards aseptic techniques, the current rare occasion of serving infection in the aesthetic environment may become a common occurrence; particularly due to the increasing popularity of many day-to-day aesthetic procedures.
REFERENCES:
1. Hassouneh B, Newman JP. Lasers, fillers, and neurotoxins: avoiding complications in the cosmetic facial practice. Facial Plast Surg Clin North Am 2013; 21: 585–98.
2. Kulichova D, Borovaya A, Ruzicka T et al. Understanding the safety and tolerability of facial filling therapeutics. Expert Opin Drug Saf 2014; 13: 1 215–26.
3. Hotta, T. A. (2018). Attention to Infection Prevention in Medical Aesthetic Clinics. Plastic Surgical Nursing, 38(1), 17–24.
4. Collier, H. (2014). The role of bacterial biofilms in aesthetic medicine: prioritising prevention. Journal of Aesthetic Nursing, 3(10), 476–481.
5. Jourdan, M., et al. Skin Care Management For Medical And Aesthetic Procedures To Prevent Scarring. Clin Cosmet Investig Dermatol. 2019; 12: 799–804.
6. Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010 Mar; 89(3):219-29.
7. Thiruvoth F., et al. Current concepts in the physiology of adult wound healing. Plastic Aesthetic Res. 2015;2:5.
8. Wand ME, Bock LJ, Bonney LC, Sutton JM. Mechanisms of increased resistance to chlorhexidine and cross-resistance to colistin following exposure of klebsiella pneumoniae clinical isolates to chlorhexidine. Antimicrob Agents Chemother 27;61(1). Pii:e01162-16.
9. Robson MC, Payne WG, Ko F, et al. Hypochlorous acid as a potential wound care agent: part ii. stabilized hypochlorous acid: its role in decreasing tissue bacterial bioburden and overcoming the inhibition of infection on wound healing. J Burns Wounds 2007. 6(e6).
10. Day A, Alkhalil A, Carney BC, Hoffman HN, Moffatt LT, Shupp JW. Disruption of Biofilms and Neutralization of Bacteria Using Hypochlorous Acid Solution: An In Vivo and In Vitro Evaluation. Adv Skin Wound Care. 2017;30(12):543‐551.
11. Rohrich RJ, Monheit G, Nguyen AT et al. Soft-tissue filler complications: the important role of biofilms. Plast Reconstr Surg. 2010; 125: 1 250–6.
12. Tortora GJ, Funke BR, Case CL. Microbiology: an introduction. San Francisco, Calif. Pearson Benjamin Cummings; 2010, 10th ed.
13. Carling PC., et al. Healthcare Environmental Hygiene Study Group. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infect Control Hosp Epidemiol. 2008;29:1-7.